Examining Protein Domains For Targeted Biologic Drug Delivery
By Robert Gensure, MD, Ph.D., BiologicsMD and Tufts University
The use of individual protein domains that have been well characterized to create hybrid proteins with desired combinations of biochemical properties is a promising new approach to biologic pharmaceutical agents.
Research in proteins of non-human origin can be of use in designing hybrid proteins, as it expands the pool of known protein domains with desired properties, and such protein domains are less likely to disrupt the function of native proteins. The bacterial collagenase COLH1 allows bacteria to spread through collagen planes. The collagenase’s specificity to cut collagen fibrils comes from its ability to bind to triple helical collagen and concentrate the collagenase activity at its intended target. The collagenase prefers to bind to disrupted helical structures, but aside from this it binds nonspecifically without an amino acid recognition sequence.1 The collagen binding activity and proteinase activity are provided by distinct domains of the collagenase, and the collagen binding domain (CBD) has been characterized.2 This CBD can thus serve as an excellent delivery system for drugs that act near collagen-containing tissues.
One example of this is the parathyroid hormone (PTH), which has important roles in regulation of calcium and bone and is an approved therapy for osteoporosis.3 It has challenges for clinical application, however, in that it is an injected medication, has a short half-life so must be given daily, and can cause hypercalcemia/hypercalciuria, risking nephrocalcinosis and kidney stone formation.4 Targeting delivery of parathyroid hormone to the intended tissues while minimizing exposure of the kidneys to the hormone’s effect could increase efficacy and duration of action and reduce side effects for PTH-based therapies. To accomplish this, a new technique uses protein domains as cassettes to create hybrid proteins with the desired properties.
Using Protein Domains As Cassettes & Targeting Delivery To Bone
The structure and functional properties of PTH are well known. It and its related protein, PTH-related peptide (PTHrP), both interact with a common receptor, the PTH/PTHrP receptor, for their biological effects. The two peptides share significant homology in the first 33 amino acids (N-terminal region) but diverge after that. N-terminal portions of PTH and PTHrP are currently utilized in treatment of osteoporosis. The function of the remaining portion of the PTH peptide is less well understood but likely has a different receptor that functions in bone formation.5 Importantly, there are no interactions or proximity between PTH and the PTH-PTHrP receptor beyond position 33; the remainder of the PTH protein appears to be free-floating when bound to the PTH-PTHrP receptor.6 Thus, the domain consisting of PTH(1-33) can be utilized to achieve PTH-like effect, even with other protein domains attached to the C-terminal of this peptide. The N-terminal region of PTH is embedded in the transmembrane region when bound to the PTH/PTHrP receptor, and any extension of PTH in this region prevents receptor activation. In fact, N-terminal extension or modification of PTH converts it from an agonist to an antagonist.7
Targeted delivery of PTH to bone has the potential to increase its efficacy, prolong its activity, and reduce the side effect of hypercalcemia by reducing serum drug levels. We prepared constructs of PTH(1-33) and the CBD from bacterial COLH1 collagenase to create a collagen-target version of parathyroid hormone. Knowing that C-terminal extensions are tolerated for PTH(1-33) and that N-terminal extensions are tolerated for CBD, we directly linked the two protein domains in this fashion. A short glycine chain was inserted to prevent any structural interactions between PTH(1-33) and CBD that could alter the function of either domain. For example, it is known that altered helicity in the C-terminal region of PTH(1-34) alters receptor interaction.8
The resulting peptide, PTH-CBD, was then tested for its biochemical properties. PTH-CBD retains its capacity to activate the PTH-PTHrP receptor, similar to that of PTH(1-34).9 It was also shown to bind collagen using flow-through assays.9 Radiolabeled PTH-CBD distributed to bone as predicted, after either subcutaneous or intraperitoneal injection, in particular to cortical bone. In-vivo testing showed that PTH-CBD increases bone mineral density,9 and micro-CT studies showed that most of this increase occurred in the cortical compartment.10 The duration of effect was one to six months after single subcutaneous injection, and there was no observed hypercalcemia. The increase in bone density was comparable to that of PTH(1-34) injected daily.
Further Investigation Yields Another Benefit
The distribution studies showed even greater distribution to skin, a tissue that is very rich in triple-helical collagen. While PTH does not have any known effects in the skin, PTHrP is produced in abundance in skin and has effects that include differentiation of keratinocytes11 and increased production of beta-catenin in hair follicles.12 Multiple injections of PTH agonists and antagonists showed effects on hair growth and cycling of hair follicles in models of chemotherapy-induced alopecia.13 Importantly, studies designed to evaluate effects of PTH-CBD in chemotherapy-induced osteoporosis also showed improvements in hair growth patterns in treated vs. control animals, with less hair loss and less hair depigmentation.14 Further investigation indicated a likely mechanism for these effects. PTH-CBD increases production of beta-catenin in bulge cells of the hair follicle,12 and increased beta-catenin initiates the hair cycle by causing the hair follicle to transition to the anagen, or growth, phase.15
We next sought other models for hair loss to investigate PTH-CBD effects on hair regrowth. Androgenetic alopecia results from testosterone’s effect to decrease beta-catenin levels in hair follicle bulge cells, but there are no available animal models for testing. Alopecia areata is caused by an autoimmune attack on anagen hair follicles, and it has a good animal model, the C3H/HeJ engrafted mouse. Testing of PTH-CBD given by single injection or weekly resulted in a marked increase in anagen hair follicles and maintenance or regrowth of hair in this model in approximately 80% of treated mice over an eight-week period.16 Again, there was no observed hypercalcemia. Currently, there is only one approved treatment for alopecia areata, a powerful immune suppressant, baricitinib.17 PTH-CBD has promise as an alternative therapy to promote hair growth without risk for serious side effects seen with immunosuppressants.
Conclusion
PTH-CBD represents the end product of decades of basic research into the functional domains of parathyroid hormone and the bacterial collagenase COLH1, regulation of bone mass, and regulation of the hair cycle. By utilizing the known structural information for parathyroid hormone and the collagen binding domain of the COLH1 collagenase, we were able to produce, using recombinant DNA technology, a hybrid peptide that binds collagen and activates the PTH/PTHrP receptor. While this peptide was designed for use as an osteoporosis treatment, we found even greater effects in the skin, promoting hair growth.
We paired a protein domain with desired biological effects with another protein domain to provide targeted delivery, thus maximizing efficacy and duration of action, while also improving the safety profile of the resulting drug agent. The use of individual protein domains that have been well characterized to create hybrid proteins with desired combinations of biochemical properties is thus a promising new approach in the design of biologic pharmaceutical agents.
References
- Philominathan ST, Koide T, Matsushita O, Sakon J. Bacterial collagen-binding domain targets undertwisted regions of collagen. Protein Sci. 2012 Oct;21(10):1554-65. doi: 10.1002/pro.2145. PMID: 22898990
- Sagaya Theresa Leena Philominathan, Takaki Koide, Kentaro Hamada, Hiroyuki Yasui, Soenke Seifert, Osamu Matsushita, Joshua Sakon. J Biol Chem. 2009 Apr 17;284(16):10868-76. doi: 10.1074/jbc.M807684200. Epub 2009 Feb 10. Unidirectional binding of clostridial collagenase to triple helical substrates.
- Forteo approved for osteoporosis treatment. FDA Consum. 2003 Mar-Apr;37(2):4. PMID: 12715752
- Ayasreh N, Fernandez-Llama P, Lloret MJ, Da Silva I, Ballarín J, Bover J. Recombinant PTH associated with hypercalcaemia and renal failure. Clin Kidney J. 2013 Feb;6(1):93-95. doi: 10.1093/ckj/sfs148. Epub 2012 Nov 15. PMID: 27818760
- P Divieti 1, N Inomata, K Chapin, R Singh, H Jüppner, F R Bringhurst. Receptors for the carboxyl-terminal region of pth(1-84) are highly expressed in osteocytic cells. Endocrinology. 2001 Feb;142(2):916-25. doi: 10.1210/endo.142.2.7955.
- Gensure RC, Gardella TJ, Jüppner H. Multiple sites of contact between the carboxyl-terminal binding domain of PTHrP-(1--36) analogs and the amino-terminal extracellular domain of the PTH/PTHrP receptor identified by photoaffinity cross-linking. J Biol Chem. 2001 Aug 3;276(31):28650-8. doi: 10.1074/jbc.M100717200. Epub 2001 May 16. PMID: 11356832
- Jonsson KB, John MR, Gensure RC, Gardella TJ, Jüppner H. Tuberoinfundibular peptide 39 binds to the parathyroid hormone (PTH)/PTH-related peptide receptor, but functions as an antagonist. Endocrinology. 2001 Feb;142(2):704-9. doi: 10.1210/endo.142.2.7945. PMID: 11159842
- Shimizu N, Guo J, Gardella TJ. Parathyroid hormone (PTH)-(1-14) and -(1-11) analogs conformationally constrained by alpha-aminoisobutyric acid mediate full agonist responses via the juxtamembrane region of the PTH-1 receptor. J Biol Chem. 2001 Dec 28;276(52):49003-12. doi: 10.1074/jbc.M106827200. Epub 2001 Oct 16. PMID: 11604398
- Ponnapakkam T, Katikaneni R, Miller E, Ponnapakkam A, Hirofumi S, Miyata S, Suva LJ, Sakon J, Matsushita O, Gensure RC. Monthly administration of a novel PTH-collagen binding domain fusion protein is anabolic in mice. Calcif Tissue Int. 2011 Jun;88(6):511-20. doi: 10.1007/s00223-011-9485-1. Epub 2011 Apr 22. PMID: 21512758
- Ponnapakkam T, Katikaneni R, Sakon J, Stratford R, Gensure RC. Treating osteoporosis by targeting parathyroid hormone to bone. Drug Discov Today. 2014 Mar;19(3):204-8. doi: 10.1016/j.drudis.2013.07.015. Epub 2013 Aug 6. PMID: 23932952
- Foley J, Longely BJ, Wysolmerski JJ, Dreyer BE, Broadus AE, Philbrick WM. PTHrP regulates epidermal differentiation in adult mice. J Invest Dermatol. 1998 Dec;111(6):1122-8. doi: 10.1046/j.1523-1747.1998.00428. PMID: 9856827
- Wysolmerski JJ, Broadus AE, Zhou J, Fuchs E, Milstone LM, Philbrick WM. Overexpression of parathyroid hormone-related protein in the skin of transgenic mice interferes with hair follicle development. Proc Natl Acad Sci U S A. 1994 Feb 1;91(3):1133-7. doi: 10.1073/pnas.91.3.1133. PMID: 7508121
- Peters EM, Foitzik K, Paus R, Ray S, Holick MF. A new strategy for modulating chemotherapy-induced alopecia, using PTH/PTHrP receptor agonist and antagonist. J Invest Dermatol. 2001 Aug;117(2):173-8. doi: 10.1046/j.0022-202x.2001.01410. PMID: 11511291
- Katikaneni R, Ponnapakkam T, Suda H, Miyata S, Sakon J, Matsushita O, Gensure RC. Treatment for chemotherapy-induced alopecia in mice using parathyroid hormone agonists and antagonists linked to a collagen binding domain. Int J Cancer. 2012 Sep 1;131(5):E813-21. doi: 10.1002/ijc.27379. Epub 2012 Jan 24. PMID: 22130912
- Huelsken J, Vogel R, Erdmann B, Cotsarelis G, Birchmeier W. beta-Catenin controls hair follicle morphogenesis and stem cell differentiation in the skin. Cell. 2001 May 18;105(4):533-45. doi: 10.1016/s0092-8674(01)00336-1. PMID: 11371349
- Katikaneni R, Gulati R, Suh D, Sakon J, Seymour A, Ponnapakkam T, Gensure R. Therapy for alopecia areata in mice using parathyroid hormone agonists and antagonists, linked to a collagen-binding domain. J Investig Dermatol Symp Proc. 2013 Dec;16(1):S61-2. doi: 10.1038/jidsymp.2013.25. PMID: 24326563
- Ali E, Owais R, Sheikh A, Shaikh A. Olumniant (Baricitinib) oral tablets: An insight into FDA-approved systemic treatment for Alopecia Areata. Ann Med Surg (Lond). 2022 Jul 13;80:104157. doi: 10.1016/j.amsu.2022.104157. eCollection 2022 Aug. PMID: 36045780
About The Author:
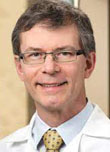 Rob Gensure, MD, Ph.D., joined BiologicsMD as chief medical officer in 2009. He is an inventor and is chief of pediatric endocrinology at Tufts University School of Medicine in Boston. He is board certified in pediatric endocrinology and pediatrics. Gensure graduated from Tulane University School of Medicine and completed his residency at Massachusetts General Hospital.
Rob Gensure, MD, Ph.D., joined BiologicsMD as chief medical officer in 2009. He is an inventor and is chief of pediatric endocrinology at Tufts University School of Medicine in Boston. He is board certified in pediatric endocrinology and pediatrics. Gensure graduated from Tulane University School of Medicine and completed his residency at Massachusetts General Hospital.
