ADC Executive Roundtable — Exploring Linker Technology
A conversation with Philipp Spycher, Daniel J. O'Connor, and Radek Špíšek
This is the second part of a series exploring antibody-drug conjugates, the science, and the potential they hold with three biopharma chief executive officers, Daniel J. O’Connor of Ambrx, Philipp Spycher of Araris, and Radek Špíšek of SOTIO Biotech.
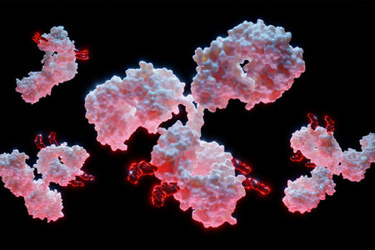
In antibody-drug conjugates, or ADCs, the linker plays an outsize role in how this emerging modality works.
The linker isn’t simply a trailer hitch. In many ways, it’s more like the driver. It decides when to release the drug and shields it from the immune system on the route to cancer cells. Optimized linker technology means the therapies reach their target and — perhaps most exciting — produce fewer off-target effects, if any.
In part one of this series, we explored advances in drug-antibody ratio technology and touched on the unsettled regulatory environment. But from where we sit, the industry appears to be putting even greater resources behind linker improvement. With that in mind, I asked our CEO panel for a status update on linkers and what’s on the horizon.
Bioprocess Online: What is the industry doing to overcome off-target toxicity?
Spycher: Limiting off-target toxicity is crucial to improving the therapeutic index of ADCs, a characteristic that has held them back from making significant progress in the clinic. A substantial contributing factor to off-target toxicity is the premature release of the payload during circulation due to unstable coupling chemistry or enzymatic linker cleavage in non-targeted tissues.
Therefore, finding the right linker that carefully balances stability in circulation, is not readily cleaved but efficiently releases the payload at the tumor, is a major goal for the industry.
Additionally, controlling the hydrophilicity of the ADCs is important to avoid non-targeted uptake in healthy tissues and maximize ADC exposure.
Špíšek: Linker stability has been improved greatly since first generation ADCs, largely reducing rapid uncontrolled release. In addition, there have been improvements in designing cleavable linkers that are cleaved by enzymes preferentially expressed in tumors, resulting in a more specific payload release inside the cancer cells. However, off-target toxicity still occurs, and some of it is attributable to the payload, known as class effect. These are monitored closely during clinical testing and, depending on the class toxicity, either preventative medication or dose and scheduling adaptations are needed to address these effects.
O’Connor: The most remarkable advancement that the industry is making to overcome off-target toxicity is the innovation occurring in ADC linkage technology that permits site-specific conjugation of antibodies to drug payload, allowing for stable delivery and controlled release of the cytotoxic drug within target cells. Additionally, improved understanding of tumor biology and the identification of specific cancer biomarkers, such as PSMA and HER2, enable the design of therapies that selectively target cancer cells based on their unique characteristics.
Bioprocess Online: We’re going to talk about drug-antibody ratios later, so let’s focus on other ways to improve conjugation. Talk about your company’s work with payloads and cell lines. Where have you found success?
Spycher: Our preclinical studies have demonstrated our ability to conjugate anticancer payloads to native antibodies in one step to generate well-defined and highly stable ADCs. For example, we demonstrated, in in vivo head-to-head studies for two different cell lines, equal efficacy at half the ADC dose versus Polivy. Additional head-to-head studies versus Padcev in a breast cancer model demonstrated complete tumor regression that lasted until the entirety of the study at a payload dose three times lower than Padcev. We are encouraged by our preclinical results showing that our ADCs are highly efficacious, even at low DAR, and well tolerated, possibly providing a more effective and better-tolerated ADC option for patients.
Špíšek: The most used payload categories are tubulin binders, topoisomerase 1 inhibitors, and DNA-targeting agents. It is important to understand that not all tumor types will be sensitive to a given type of payload and, in this context, the selection of appropriate cell lines and models is critical in the evaluation of the drug candidates. Regarding the payloads and cell lines, we are paying attention to the mechanism of action of the payloads and potential multidrug resistance (MDR) proteins expressed in the cancer cells.
Some of the payloads, like MMAE, are known substrates for such proteins. And conversely, some of the indications and cell lines are known to have high expression of MDR proteins, exemplified by the expression of the multidrug resistance protein 1 in most melanomas. Such pairing can result in reduced efficacy that can be observed in both in vitro and in vivo models. We also need to take into consideration the current standard of care (SoC) for the patients and how that might affect our ADCs. The key is to avoid added toxicities. Therefore, selecting suitable payloads for the considered indication is key, and in our preclinical programs, we are actively focusing on this.
O’Connor: Ambrx is developing an expanded genetic code technology platform for incorporation of synthetic amino acids (SAA) into proteins at selected sites in industry-standard cell lines. The result is product candidates specifically engineered to overcome the inherent limitations of conventional conjugation approaches that use natural amino acids without control of what site to conjugate — offering potential safety and efficacy benefits to patients. The incorporation of SAAs enables proprietary, highly stable oxime conjugation that differs from other ADCs reliant on conjugation that can only be placed at cysteines or lysines. With the full exclusive license from The Scripps Research Institute, Ambrx’s scientists and protein engineers have honed the technology and created the only mammalian expression system in the industrial setting.
AS269, our proprietary payload, is a tubulin inhibitor specifically designed to form a highly stable covalent bond with our SAAs and kill tumor cells only upon entry into the cell via the conjugated targeting antibody. The resulting conjugation is highly stable; we only detect a single metabolite from the ADC, pAF-AS269 (our SAA covalently connected with our linker plus cytotoxic payload), in nonclinical and clinical studies.
Bioprocess Online: What are some big linkage challenges you want to overcome in the next five to 10 years? Likewise, what’s your strategy to do it?
Spycher: The linker is crucial to the success of the ADC by delivering the payload to its targeted site while avoiding premature payload loss due to unstable coupling chemistry or enzymatic linker cleavage in non-targeted tissues. Identifying linkers with an improved and highly controlled payload release profile in targeted tissues would launch ADCs to new heights.
At Araris, we have been developing our own proprietary linker technology that has demonstrated compelling stability in all animals tested, including monkeys, with superior efficacy and tolerability to approved ADC therapeutics. Since we are relying on peptidic linker structures we can screen for linkers that show the least toxic profiles in certain tissues and potentially generate ADCs with reduced dose-limiting toxicities like neutropenia or peripheral neuropathy. This is one of our strengths — the ability to select for the best possible linker. We’ve found that ADCs are not plug-and-play and there is no such thing as a one-size-fits-all linker. In addition, our linker technology enables payload conjugation to off-the-shelf antibodies, meaning no additional antibody engineering is required.
Špíšek: SOTIO Biotech is utilizing what we consider third-generation ADC technology provided to us by our platform partners. These ADCs employ site-specific conjugation methods resulting in homogeneous and reproducible ADCs with improved stability and pharmacokinetic (PK) properties.
The aim is to widen the therapeutic window, and this is what we have been seeing in our preclinical models when compared to second-generation benchmark ADCs. However, there is still room for linker optimization. For example:
- We know linkers can have negative effects on absorption, distribution, metabolism, and excretion (ADME) properties.
- There’s a consensus that hydrophilic ADCs are more effective than hydrophobic ones, so we need strategies for improving the hydrophilicity.
- Linkers can also affect payload kinetics in tumors, so plasma pharmacokinetics of the conjugated and unconjugated ADC should be monitored in relevant models as part of preclinical development.
- Increased hydrophilicity can also reduce nonspecific liver absorption, thus reducing off-target toxicity.
- Currently, both non-cleavable and cleavable linkers are being clinically developed and approved. More efforts have focused on the latter; however, there is a need for both and thus efforts to develop non-cleavable linkers should continue.
O’Connor: ADCs have been considered a promising class of targeted cancer therapies for over 20 years, yet they have failed to live up to their full potential. In particular, ADCs that have weak linkage can prematurely release their toxic payload, which can damage healthy tissues and lead to an unacceptable toxicity profile. Ambrx is addressing the current limitations of traditional conjugation with our proprietary conjugation technology that minimizes the premature release of cancer-killing toxic payloads, achieving efficient elimination of cancer cells with limited off-target effects. We have already observed initial patient benefits in clinical trials, and in the next five to 10 years we will continue advancing our clinical-stage portfolio so that ADCs with stable conjugation technologies become widely available to physicians and patients.
About the Experts:
 Daniel O’Connor has over 23 years of executive experience and leadership in all aspects of the biopharmaceutical industry, including CEO leadership of two public oncology-focused companies, OncoSec Medical and Advaxis Inc., and other executive leadership roles at ImClone Systems, Bracco Diagnostics, and the former PharmaNet Inc., now Syneos Health. He has led numerous life sciences licensing transactions and drug development collaborations with major pharmaceutical companies and has raised hundreds of millions in the capital marketplace. He earned a J.D. from the Dickinson School of Law of Pennsylvania State University and a B.A. from Boston University.
Daniel O’Connor has over 23 years of executive experience and leadership in all aspects of the biopharmaceutical industry, including CEO leadership of two public oncology-focused companies, OncoSec Medical and Advaxis Inc., and other executive leadership roles at ImClone Systems, Bracco Diagnostics, and the former PharmaNet Inc., now Syneos Health. He has led numerous life sciences licensing transactions and drug development collaborations with major pharmaceutical companies and has raised hundreds of millions in the capital marketplace. He earned a J.D. from the Dickinson School of Law of Pennsylvania State University and a B.A. from Boston University.
 Radek Špíšek graduated from the First Faculty of Medicine of Charles University in Prague and received his Ph.D. in immunology. Between 2000 and 2002, he worked at Institute de Biologie of Université de Nantes in France. He spent 2005 to 2007 on the team led by Professor Ralph Steinman, a medicine and physiology Nobel laureate, at the Laboratory of Cellular Physiology and Immunology/Center for Immunology and Immune Diseases, Rockefeller University, New York. He focuses on tumor immunology and tumor immunotherapy. He is a professor at Charles University’s Second Faculty of Medicine. He has received postgraduate clinical certification in pediatrics and in allergology and clinical immunology. He joined SOTIO in 2010 where he has been a member of the company’s management and has overseen research and manufacturing. He was appointed CEO in March 2018.
Radek Špíšek graduated from the First Faculty of Medicine of Charles University in Prague and received his Ph.D. in immunology. Between 2000 and 2002, he worked at Institute de Biologie of Université de Nantes in France. He spent 2005 to 2007 on the team led by Professor Ralph Steinman, a medicine and physiology Nobel laureate, at the Laboratory of Cellular Physiology and Immunology/Center for Immunology and Immune Diseases, Rockefeller University, New York. He focuses on tumor immunology and tumor immunotherapy. He is a professor at Charles University’s Second Faculty of Medicine. He has received postgraduate clinical certification in pediatrics and in allergology and clinical immunology. He joined SOTIO in 2010 where he has been a member of the company’s management and has overseen research and manufacturing. He was appointed CEO in March 2018.
 Philipp Spycher has an extensive background in bioconjugation and ADCs. He obtained his master’s degree and Ph.D. from ETH Zurich in material science and protein engineering. During his post-doctoral work at Paul Scherrer Institute, he introduced the novel approach of using transglutaminases for antibody conjugation, which led to the discovery of what is now called Araris linker technology.
Philipp Spycher has an extensive background in bioconjugation and ADCs. He obtained his master’s degree and Ph.D. from ETH Zurich in material science and protein engineering. During his post-doctoral work at Paul Scherrer Institute, he introduced the novel approach of using transglutaminases for antibody conjugation, which led to the discovery of what is now called Araris linker technology.
