Overcoming The Unique Filling Challenges Of Autologous Therapies
By Herman F. Bozenhardt and Erich H. Bozenhardt
 Autologous (patient-derived) therapies represent unique challenges to processing. One-patient, single-batch is a radical change from the scale our industry is accustomed to. At this level the filling is more analogous to limited Phase 1 clinical trial materials or even preclinical applications. The logistics and required compliance of manufacturing these personalized therapies is drastically different and presents a combinatorial explosive problem. One aspect of this process where traditional methods fall apart is filling of these therapies.
Autologous (patient-derived) therapies represent unique challenges to processing. One-patient, single-batch is a radical change from the scale our industry is accustomed to. At this level the filling is more analogous to limited Phase 1 clinical trial materials or even preclinical applications. The logistics and required compliance of manufacturing these personalized therapies is drastically different and presents a combinatorial explosive problem. One aspect of this process where traditional methods fall apart is filling of these therapies.
While the presentations for these therapies vary depending on the ultimate administration, bags and vials are the most commonly used forms of containers. There are industry-proven solutions for small-scale vial filling, but personalized therapies redefine small scale. Clinical lots for traditional therapies are in the low-hundreds vial range, but for autologous filling the lot might be only be a handful of vials.
A research scientist would typically hand-fill a set of 10 vials for sample analysis or to send to their animal study. This is done with less-than-GMP aseptic care, because the focus is on a quick turnaround for analysis and only a specific, defined outcome. The patient at this stage is a brave rodent.
In this R&D model, we have the characteristics of manual filling, single-operator mode, biosafety cabinets, hand-labeling, and hand-delivery into the shipping container.
Taking our pharmaceutical methods and mindset from a few hundred vials to a handful requires thinking in discrete units rather than a continuous feed of vials. For example, a batch might be a 50 ml unit of product for sale and four 5 ml vials for samples and retains. With a batch of five vials in mind, the typical approach of filling with pipettes in a biosafety cabinet seems to fit. The challenge is the open, manual nature of this process represents serious risks for sterility and uniformity, particularly as the number of batches increases during the product’s transition from clinical trials to commercial scale. Closed-vial filling allows the flexibility of hand-filling but adds a layer of sterility protection during the filling operation. This is ideal, as the setup, weight checks, fill, and cleanup are very simple. The cleanup is, in fact, tear out and throw away.
The vials for closed-vial filling are also typically plastic, in particular cyclic olefin copolymer, allowing cryogenic freezing. Traditional glass vials with rubber stoppers have been shown to have seal integrity concerns at cryogenic temperatures and should be avoided if possible, for cryogenic applications.1 (For a deeper dive into manual filling, read “Manual Aseptic Processing: The Last Resort Or The Best Approach?”)
Other possibilities for filling that have not been explored sufficiently could be adapted. These include R&D liquid-handling systems (e.g., Hamilton Microlab STAR, Hudson Robotics SOLO, Eppendorf epMotion, etc.), which use robots to dispense micro-quantities into various polymer cells and vessels. The new generation of pharmaceutical robotic filling systems are very adept at filling 1 to 50 ml with excellent accuracy. They are built to fill nests of 60 to 100 vials or syringes. These systems could be adapted to include a front-end robot to remove the incoming nest’s covers and provide sterile handling of nests as small as 20 vials. In addition, the system should include a back-end robot to remove the nest automatically, label it, and serialize it.
Since the therapies are typically infused, bags that can be directly attached to an IV set are a common option for autologous therapies. The best practice is to fill volumetrically using a closed system driven by a peristaltic pump with a weight check of the filled units. Bags are typically loaded into cassettes (see Figure 1) to provide a uniform thickness for freezing and to protect the bag from mechanical damage. Even bags with films designed for cryogenic temperatures become more damage-prone at those temperatures.
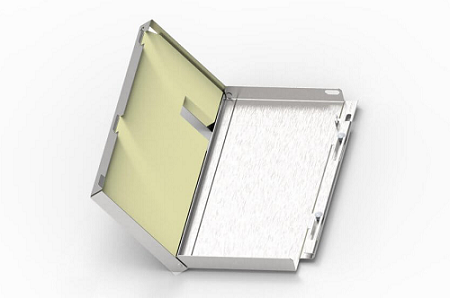
Figure 1: Example cassette (image courtesy of SUSupport)
Inspection and labeling typically coincide with filling. This avoids the intermediate bright stock tracking challenges and can allow for quicker processing. The processing time between formulation and cooling/freezing is typically a critical process parameter and can be only a few hours.
Due to the low throughput (as most autologous therapies are still in clinical trials), operators cover the whole process and do not specialize in particular unit operations. Typically, the operators are converted development scientists. As these processes expand in scale and diversity, it may become more efficient for people to specialize in particular unit operations and operators may not need be as technically deep as the current generation. Aseptic filling is a high-risk process and frequently done under tight time constants due to product stability, thus the need for more automation and a robotic filling system if possible. A method for real-time deviation management is needed. Currently companies have been physically co-locating production facilities with research and development, but that doesn’t make sense in the long-term supply chain. That also positions the facility to be vulnerable to GMP violations, as the practices from R&D may be carried over into the GMP production and found to be noncompliant.
Managing the process and having an autonomous master batch record is required. Developing and editing batch records with minor changes and the typically extensive review process is time-consuming and clumsy for today’s level of technology and the therapy’s life span. Part of the solution for the batch record is an automated electronic system with each patient’s requirements queued up in it.
After that, written or automated troubleshooting flowcharts are a key to managing deviations in real time. Exceptions or deviations, whether smudged initials on the batch record or a missing vial label, can cause serious time delays in the process as well as compliance issues. The primary reasons for this are the bulk of the operations are executed by one pair of operators throughout the process, the technology is new to all manufacturers, and the expertise to solve all problems is not readily available. This is an ideal application for artificial intelligence (AI). In the 1990s, the U.S. Army created an onboard, AI-based diagnostic system for its Abrams tank because the detailed expert knowledge could not be retained in every tank crew. The core of the system was its ability to provide an expert flowchart and specific diagnostic path for problems as they occurred. We believe AI capability is needed in this application to keep operators productive and not bog them down with finding out the mechanism to solve a problem, let alone solve it. This AI system could be built with an object-oriented development “shell” or a simple frame system, which would allow it to be validated and 21 CFR Part 11-compliant. Therefore, whether the problem was a documentation omission or a weight check problem in the filling process, the system would provide a step-by-step flowchart or text-based instructions on the expert way to solve the problem, close the deviation, or resolve the issue.
Autologous filling represents many unique challenges to processing. One-patient, one-batch redefines the industry’s understanding of small-batch filling, but established practices can be leveraged to overcome some of these challenges. As more personalized medicine therapies transition from clinical to commercial scale, a new specialization in the industry will have to develop best practices. Until then, we need to share methods and technologies from across the R&D space, pharmaceutical manufacturing, and manufacturing of semiconductors and other precision and technical products.
References:
- Winters, Whitney. “Biologics: When Glass Fails At Low Temperatures, Consider A Cyclic Olefin Polymer System.” https://www.pharmaceuticalonline.com/doc/when-glass-vials-fail-at-low-temperatures-consider-a-cyclic-olefin-polymer-system-0001
About The Authors:
 Herman F. Bozenhardt has 42 years of experience in pharmaceutical, biotechnology, and medical device manufacturing, engineering, and compliance. He is a recognized expert in aseptic filling facilities and systems and has extensive experience in the manufacture of therapeutic biologicals and vaccines. His current consulting work focuses on aseptic systems, biological manufacturing, and automation/computer systems. He has a B.S. in chemical engineering and an M.S. in system engineering, both from the Polytechnic Institute of Brooklyn. You can reach him via email at hermanbozenhardt@gmail.com and connect with him on LinkedIn.
Herman F. Bozenhardt has 42 years of experience in pharmaceutical, biotechnology, and medical device manufacturing, engineering, and compliance. He is a recognized expert in aseptic filling facilities and systems and has extensive experience in the manufacture of therapeutic biologicals and vaccines. His current consulting work focuses on aseptic systems, biological manufacturing, and automation/computer systems. He has a B.S. in chemical engineering and an M.S. in system engineering, both from the Polytechnic Institute of Brooklyn. You can reach him via email at hermanbozenhardt@gmail.com and connect with him on LinkedIn.
 Erich H. Bozenhardt is the process manager for Integrated Project Services’ process group in Raleigh, North Carolina. He has 12 years of experience in the biotechnology and aseptic processing business and has led several biological manufacturing projects, including cell therapies, mammalian cell culture, and novel delivery systems. He has a B.S. in chemical engineering and an MBA, both from the University of Delaware. You can reach him at ebozenhardt@ipsdb.com and connect with him on LinkedIn.
Erich H. Bozenhardt is the process manager for Integrated Project Services’ process group in Raleigh, North Carolina. He has 12 years of experience in the biotechnology and aseptic processing business and has led several biological manufacturing projects, including cell therapies, mammalian cell culture, and novel delivery systems. He has a B.S. in chemical engineering and an MBA, both from the University of Delaware. You can reach him at ebozenhardt@ipsdb.com and connect with him on LinkedIn.
