The CAR T Speed Show

By Matthew Pillar, Editor, Bioprocess Online
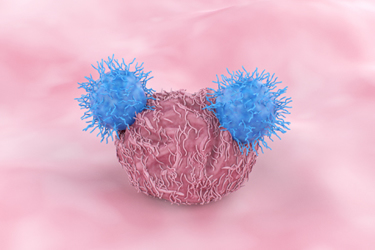
This Spring, Penn researchers from the Perelman School of Medicine at the University of Pennsylvania made quite a news splash with a pre-clinical study published in Nature Biomedical Engineering. The study demonstrated that these researchers could develop autologous CAR T-cells with enhanced anti-tumor potency in 24 hours – effectively extracting a cancer patient’s immune cells, altering them, and infusing them back into the patient—in a fraction of the current 9-to-14-day standard.
I was impressed by said splash, but it occurred to me that I’d heard this story before. More than once, in fact.
Back in March 2021, I discussed the concept with clinical-stage Precigen President & CEO Helen Sabzevari, Ph.D. on this episode of the Business of Biotech podcast. We talked at length about Dr. Sebzevari’s vision for overnight CAR T manufacturing and administration in hospital settings, facilitated by proprietary UltraPorator electroporation technology and her company’s UltraCAR-T platform.

These are exemplary of the many emerging biotechs seeking to address the problems associated with the current CAR T paradigm. The inaccessibility of a process that yields half-a-million-dollars-per-dose therapies. Too much time and too many logistics in the manufacturing process. The heterogenicity challenge. These hurdles have been enough to cause many leading minds in the CAR T game to walk away from the autologous table and put all their chips down on allogeneic approaches.
But then, Penn made this splash, effectively reinvigorating the debate.
I caught up once again with EXUMA’s Dr. Frost in advance of his company’s trip to the American Association of Cancer Research Annual Meeting in New Orleans. There, EXUMA’s mission was to present preclinical data on why its subcutaneous CAR-TaNK therapy for hematological tumors gives it a high-probability shot at being the first company to take a subcutaneous, synthetic lymph node cell therapy to clinic.
We talked about that, but the first thing I asked him was to reflect on the news out of Penn.
“People rediscover the wheel in this industry every day, but the important element is that there was some really good work done at Penn,” said Dr. Frost, before shifting quickly to the work done at EXUMA. When it began working on rPOC roughly six years ago, EXUMA was laser-focused on two pieces of the equation—manufacturing and administration.
Manufacturing CAR T-Cells In Rapid Fashion
First, EXUMA focused on lentivector manufacturing systems. “For many years, everyone—whether at NCI or MD Anderson or anywhere else work has been done on gene vector systems—knew that nothing would happen from getting a peripheral blood draw of lymphocytes, those cells circulating in the blood that are the starting material for making these cellular therapies, and simply putting a virus on them,” said Dr. Frost. “We also know that if you give them lots of cytokines and growth factors and get them dividing, then you can go about making them receptive to viral modification.”
Historically, in the academic setting, the process of activating the cells in culture, waiting as they proliferate, and then modifying them with gene vectors would take about 10 days. That ten-day manufacturing period was rational at the point of care, where patient preparation often included chemotherapy for lymphodepletion.
“But as you look at the viability of these products in a commercial distribution and supply chain context, you see a lot of cost and complexity. So, we asked, can we make these viruses a little bit smarter, so they can do the heavy lifting?”
In engineering its vectors, EXUMA looked beyond activation and division. It sought to load lymphocytes with a vector that’s directed to bind only to the cells of EXUMA’s choosing. “At the same time, in the process of the cells taking up those vectors and internalizing them, they're also getting turned on. It’s at that precise point that they’re injected subcutaneously to make these synthetic lymph nodes,” Dr. Frost explained.
Changing The CAR T Administration Paradigm
After addressing the engineering challenge, EXUMA turned its attention to patient administration. The speed at which it could process cells for administration, and the speed at which administration was necessary, it surmised, was meaningless if clinicians needed five or more days to prepare the patient with lymphodepletion. “We employed big data and analytics to screen through myriad gene components to determine what signals we could provide with the therapy, in addition to the CAR, to get them to amplify,” said Dr. Frost. “We didn’t ask a priori, ‘can we make an NK cell or a T & NK cell? We simply asked, “what cells can we amplify without lymphodepletion?’” The exercise found that the cell types EXUMA was amplifying differentiate into a phenotype that’s great for hunting down tumors, but which Dr. Frost says may do it in a gentler way than current approaches.
“We think that having these two components, and being able to rapidly load them, by simply loading the vector on the cells and slipping them under the skin, we can let the body do the rest of the work,” said Dr. Frost. “We end up making tissue that, if biopsied and examined microscopically, look like normal lymph nodes. It’s really a back door approach in some ways. Rather than just distributing these cells all over the bloodstream and hoping one of them lands in a good place, we put them all in one place under the skin so they can work better as a team.”
Mimicking Nature’s Pathology
Dr. Frost said the EXUMA approach is akin to the natural, steady, and ongoing response to pathogens, and that it enables a significantly smaller therapeutic effort—and dose—than traditional intravenous administration of cell therapies. The result, he said, is as natural as lymph nodes that swell with cell stimulation and expansion before deploying TaNK cells via the lymphatics to hunt down antigens. “We did some careful work labeling cells with gene markers so they would fluoresce. When you put these cells that have been loaded with the vector under the skin, they haven’t even integrated the gene product yet. That takes about three days. So, the first time you see the signal of the CAR-modified cells coming out is around day 4 or 5,” explained Dr. Frost. Those cells build into critical mass, and once they’re released into the blood, they show up first in the tumor, most likely from direct lymphatic access. From a pharmacokinetic standpoint, this steady and continual progression of fresh cells to the tumor site, said Dr. Frost, may be safer due to an inherent decrease in the risk of cytokine release syndrome, which can result from intravenously infusing large numbers of highly activated cells in current CAR- T cell therapies.
“We think this approach may prove more efficacious than injecting something grown in a petri dish, and we believe that the time savings factor will contribute to our success,” said Dr. Frost. “Time is the enemy of clinical trials in oncology. If we can do something in a few days that currently takes weeks—weeks the patient might not have—we think we’ll see success.”
Whether this spring’s news out of Penn is a first, or a first-of-its-kind, is up for debate and subject to a host of defining factors. What’s for sure is that it’s buoying the industry and drawing attention—and competition—to the race for fast, accessible cell therapy in oncology.
